Misdiagnosis of the bacterial skin condition cellulitis often leads to unnecessary antibiotic use and hospitalizations, a new study says.
About one-third of people diagnosed with cellulitis don’t actually have it, researchers from Brigham and Women’s Hospital in Boston found.
The researchers looked at a 30-month period, examining the medical records of 259 people hospitalized for lower extremity cellulitis in the hospital’s emergency department.
But, 79 of the patients didn’t have cellulitis. Almost 85 percent didn’t need hospitalization and 92 percent didn’t need the antibiotics they received, the researchers said.
Looking at how their findings might reflect the nation as a whole, the researchers estimated that the misdiagnosed skin condition leads to about 130,000 unnecessary hospitalizations. The problem may cause up to $515 million in unneeded medical spending each year, the researchers said.
In addition, the researchers estimated that the unnecessary antibiotics and hospitalizations may actually lead to thousands of infections, which can be deadly.
The challenge of diagnosing cellulitis is that patients may actually suffer from a condition called pseudocellulitis.
“It mimics signs and symptoms of cellulitis, which makes diagnosis difficult, especially since there are no laboratory or imaging studies that reliably differentiate the two,” Dr. Arash Mostaghimi, director of the dermatology inpatient consult service at Brigham and Women’s Hospital, said in a hospital news release.
Mostaghimi suggested that having a dermatology consultation before hospital admission could help reduce the number of misdiagnosed cases.
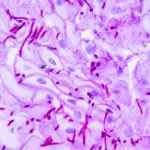
According to the U.S. National Institutes of Health, cellulitis is an infection of the skin and deep underlying tissues. Group A strep bacteria are the most common cause. The bacteria enter the body when you get an injury such as a bruise, burn, surgical cut or wound.
Symptoms include: fever and chills; swollen glands or lymph nodes; and a rash with painful, red, tender skin, the NIH says.
The study appears Nov. 2 in the journal JAMA Dermatology.
[Source:-UPI]